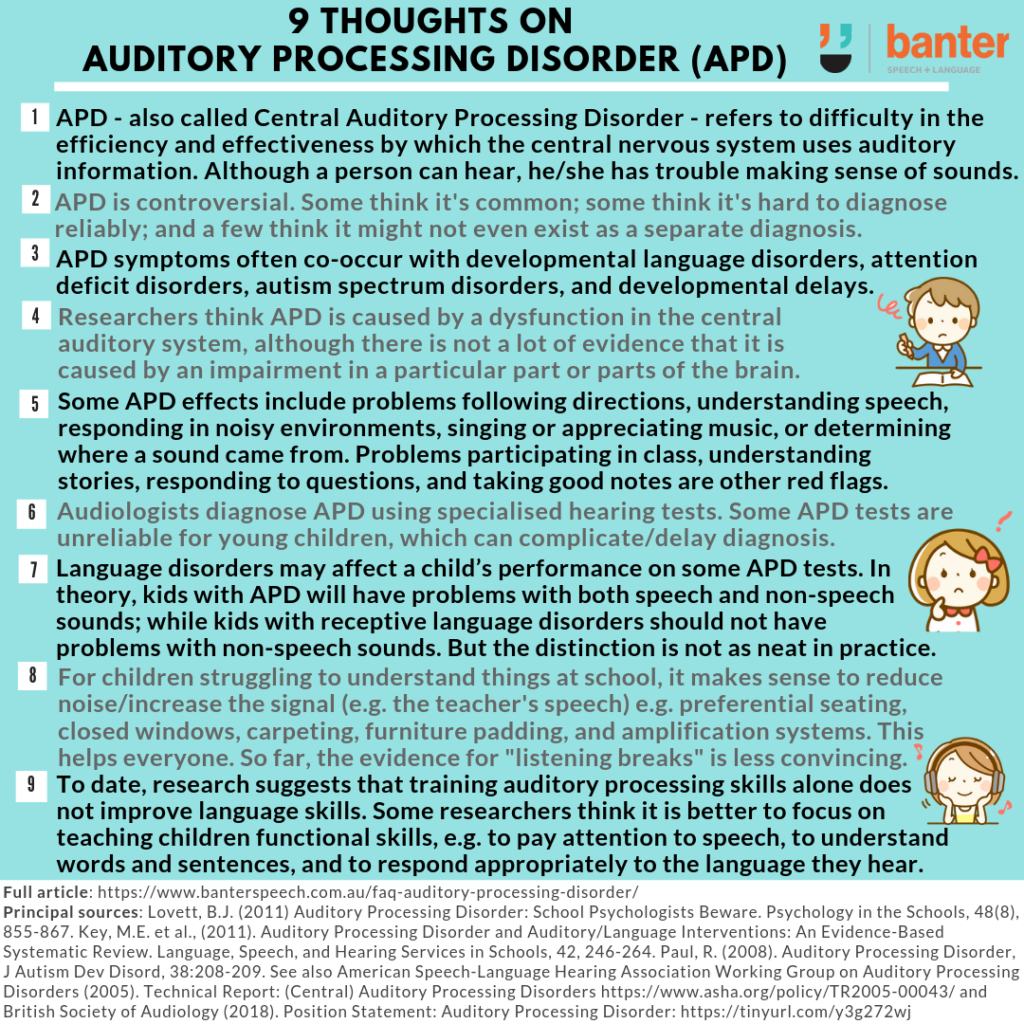
At least once a month, I get asked about auditory processing disorder (APD), which is also known as central auditory processing disorder.
APD is a controversial topic in Australia and overseas, and I write this post with some trepidation. While some studies suggest something like 2-5% of school-age kids meet the criteria for a diagnosis of APD (e.g. Bellis & Anzalone, 2008), the correct diagnosis is often hotly debated, with some researchers questioning whether it is over-diagnosed; others questioning whether it exists as a reliable diagnosis (see, e.g. Levy & Parkin, 2003) and yet others suggesting it might be a “twentieth century unicorn” (Kamhi and Beasley, 1985).
The purpose of this article is to address some basic questions about the disorder based on recent evidence, recognising that the experts have yet to reach a consensus on differentially diagnosing APD from other disorders or how best to treat it.
1. What is APD?
Auditory processing disorder is defined as a difficulty in the efficiency and effectiveness by which the central nervous system uses auditory information (e.g. ASHA, 2005).
What does this mean? It means that an individual has normal sensitivity to sounds (i.e. they can hear) but has trouble making sense of the sounds. One researcher likens APD’s features to being able to hear, “but acting as if hearing impaired” (Lovett, 2011).
2. What are its symptoms?
According to the American Academy of Audiology (2010), the most common effects of APD include problems following directions, understanding speech, responding in noisy environments, singing or appreciating music and determining where a sound came from.
At school, red flags for APD are said to include problems participating in class, understanding stories, responding to questions and taking good notes (e.g. Geffen, 2007).
3. What causes it?
APD is thought to be caused by dysfunction in the central auditory system, although there is not a lot of direct evidence that it is caused by an impairment in a particular part or parts of the brain (one reason why the word “central” has been dropped by many researchers investigating APD).
4. Who diagnoses APD and how?
Qualified audiologists diagnose APD in Australia, the US and the UK.
APD cannot be properly diagnosed unless the person has undergone specialised hearing tests using special equipment measuring the person’s ability to locate sounds, discriminate between different sounds, discriminate between similar sounds, detect small differences in the timing of sounds, the order of sounds and sound patterns, and respond to sounds that are “degraded” (e.g. by having some of their auditory information “masked”).
To receive a diagnosis, the person being tested must score at least 2 standard deviations below the average on at least two auditory processing tasks (ASHA, 2005).
5. So why the controversy?
Diagnosing APD is not as simple as it sounds (no pun intended):
- APD is a collection of symptoms that usually co-occurs with other neuro-developmental disorders (British Society of Audiology, 2011);
- Many of the symptoms and red flags for APD overlap with those seen in other disorders, including receptive language disorders (diagnosed by speech pathologists), attention deficit disorders (diagnosed by psychologists and psychiatrists), autism spectrum disorders and general developmental and cognitive delays (usually diagnosed by a multi-disciplinary team, including a paediatrician);
- Some of the hearing tests used to diagnose APD are considered unreliable for children under seven; with some considered unreliable for children under 10 years of age (Lovett, 2011). Audiologists investigating APD recognise the urgent need for more appropriate, objective tests of auditory function to serve as a “gold standard” for APD assessment (e.g. British Society of Audiology, 2011);
- Many children perform inconsistently on APD tests, and it is hard to tell whether their poor performance is caused by difficulty in transmitting sound from the ear to the brain, difficulty interpreting the sounds once they get to the brain, simply not paying attention to the sounds, not being motivated to try hard enough to make the distinctions required, or a combination of these factors (Paul, 2008);
- Receptive language delays (comprehension problems) are likely to impact adversely on a child’s performance on some of the hearing tests – particularly those that require a child to repeat words presented with background noise;
- counter-intuitively, there is no correlation between performance on auditory processing tasks and standardised measures of academic performance (e.g. Watson & Kid, 2009); and
- As the British Society of Audiology states: “There is clearly no consensus here but, rather, a list of problems that may be due to one or several causes”.
6. Is APD the same thing as a receptive language disorder?
No, though, again, there is a considerable overlap in many of the red flags and symptoms of each disorder.
In theory, the key difference is that children with APD are thought to have problems processing both speech and non-speech sounds (British Society of Audiology, 2011). Children with receptive language disorders, on the other hand, should not have problems on tests involving non-speech sounds (such as determining whether two tones are the same or different, or whether there was a gap between two different tones).
Audiologists diagnose APD only after they have tested the person’s ability to process speech and non-speech sounds. But, because of problems with the reliability of some of the APD tests (including the effects of attention and motivation on test performance), the distinction is not as neat in practice as it sounds in theory.
7. How is APD treated?
There are a few types of treatment for APD:
- Making environmental changes aimed at increasing the signal-to-noise ratio (increasing important sounds and decreasing irrelevant sounds). These treatments include preferential seating, closing windows, adding carpeting, and padding the bottom of chair legs to decrease noise. They also include amplifying important sounds (e.g. the teacher’s voice). Classroom acoustic research shows that these changes can benefit all students (including children with APD and other information processing disorders) (e.g. Crandall et al, 2005).
- Special accommodations for students with APD: these include providing students with APD with written notes and “listening breaks”, as well as extra time during tests, and testing in a separate room (to minimise noise). There doesn’t seem to be much research supporting these measures, but they are increasingly popular (in part, because they are easy and cheap to implement).
- Auditory processing skills training: the idea behind these treatments (which are often computer-based) is that giving students lots of practice with auditory processing tasks will, over time, increase their listening skills and generalise to the real world. To date, research shows that, although children get better at doing the exercises, there are very limited changes in their functional listening behaviour in real world environments. For example, in 2011, Fey and colleagues conducted a systematic review of the evidence for auditory processing interventions and concluded that there is only limited evidence supporting the use of auditory processing treatments to improve spoken or written language functioning. It should be noted that Fey’s conclusions have been challenged by other researchers, and that research continues on the effectiveness of auditory processing training.
8. Bottom line
To date, there is no consensus on a diagnostic rule detailed enough for clinicians to reliably distinguish APD from other information processing disorders, especially when other disorders such as attention deficit hyperactivity disorder and receptive language problems must be ruled out as causes of poor performance on auditory processing tests.
Having reviewed the evidence to date, I can see the clear benefit in making environmental changes in the classroom to help children diagnosed with APD (and other information processing disorders). I also agree with Rhea Paul (2008) who, in the context of talking about children diagnosed with APD and autism, concluded that it makes most sense to spend intervention time on functional activities teaching children to pay attention to speech, to learn to comprehend words and sentences, and respond appropriately to the language they hear. But we also need to keep an open mind and close eye on developments in this important space as more research is published about the effectiveness of listening treatments for APD and, in particular, their effects on real world outcomes.
Key sources:
- Lovett, B.J. (2011) Auditory Processing Disorder: School Psychologists Beware. Psychology in the Schools, 48(8), 855-867.
- Key, M.E., Richard, G.J., Geffner, D., Kamhi, A.G., Medwetsky, L., Paul, D., Ross-Swain, D., Wallach, G.P., Frymark, T., & Scooling, T. (2011). Auditory Processing Disorder and Auditory/Language Interventions: An Evidence-Based Systematic Review. Language, Speech, and Hearing Services in Schools, 42, 246-264.
- Paul, R. (2008). Auditory Processing Disorder, J Autism Dev Disord, 38:208-209.
- American Speech-Language Hearing Association Working Group on Auditory Processing Disorders. (2005). Technical Report: (Central) Auditory Processing Disorders, retrieved on 18 April 2015 from here.
- British Society of Audiology (2011). Position Statement and Practice Guidance Auditory Processing Disorder (APD), retrieved on 17 March 2019 from here.
Image: http://tinyurl.com/q9rf7us

Hi there, I’m David Kinnane.
Principal Speech Pathologist, Banter Speech & Language
Our talented team of certified practising speech pathologists provide unhurried, personalised and evidence-based speech pathology care to children and adults in the Inner West of Sydney and beyond, both in our clinic and via telehealth.


My sister’s little girl was just diagnosed with APD and I don’t really understand too well what the implications are. Thank you for clarifying that APD is usually coupled with other types of neuro-developmental disorders. This helps to understand that although the disorder itself is not the worst, there are other possibilities still out there. I will be sure to continue reading up so I know how to talk with my Sister about it.