Progress Note System (Therapy)
$10.00 including GST
In our practice, we use a progress note system. For each client, and for every session, we use a system that integrates:
-
- key therapy recommendations, including goals and dosage;
- home practice recommendations;
- data collection and progress;
- built in-breaks and discharge plans; and
- planning for the client’s next session.
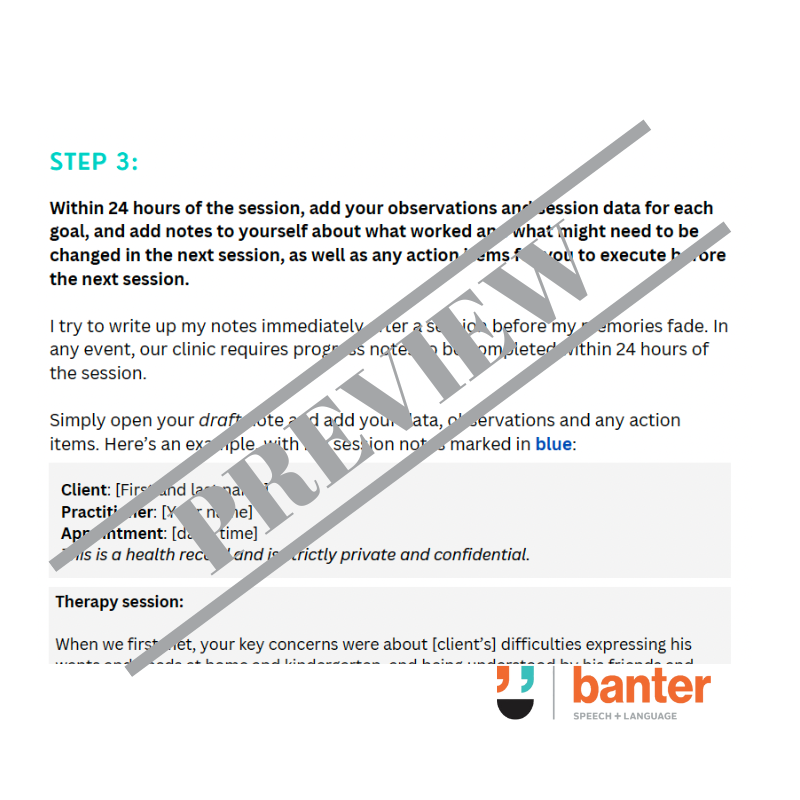
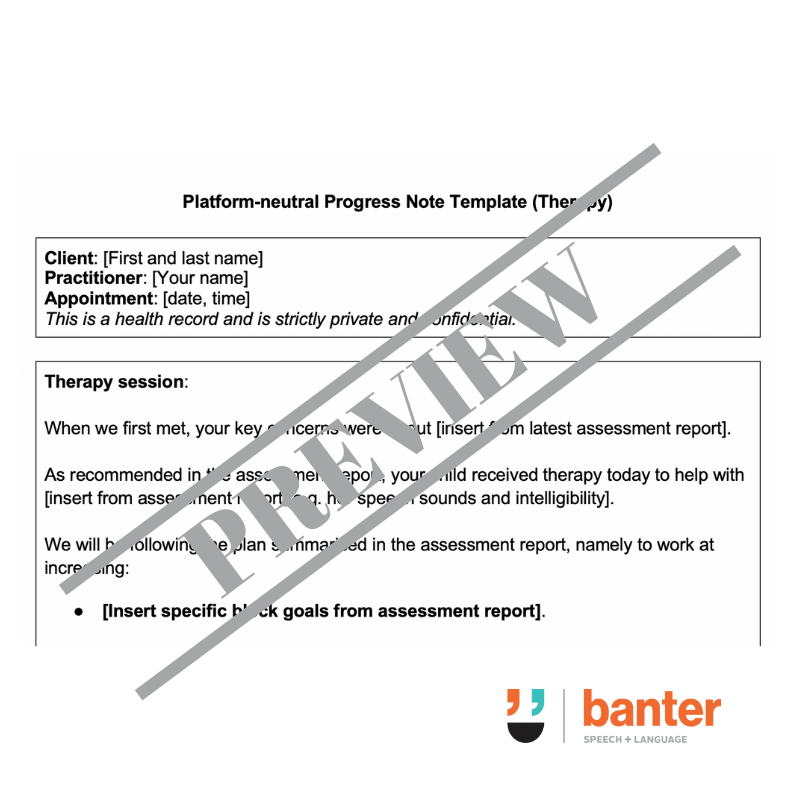
Our Progress Note System (Therapy) is available as a 15-page PDF (including a worked example) and a 2-page platform-neutral template (Word).
Description
No one likes writing progress notes – especially when you’re booked back-to-back, with calls to return, and clients waiting. But we all have to do it:
- It’s a legal obligation, e.g. under the various state statutory Codes of Conduct and health laws.
- It’s an ethical obligation, e.g. under professional Codes of Ethics.
- It’s an important risk management tool for your practice, e.g. in the event of a complaint, allegation, threatened or actual litigation, or on receipt of a subpoena.
- It’s essential for monitoring therapy outcomes.
When done well, progress notes:
- enhance your communication and partnership with clients and their families, allowing you to educate families about communication challenges and evidence-based treatment options;
- provide a framework for critical reflection and session planning;
- support family–centred care, providing a shared foundation for open discussions and troubleshooting about priorities, home practice, progress, outcomes, therapy breaks and discharge; and
- form an important part of proper supervision systems, by helping supervisors and practice owners oversee your work and the development of your clinical thinking, without micromanaging you.
Traditional progress notes – often structured around medical note-taking acronyms like ‘SOAP’ (Subjective/Situation, Objective, Assessment, and Plan) – are okay. But, in private practice clinical or mobile service settings, they are inefficient and of limited practice use – especially when dashed off, filed and forgotten. They don’t help you become a better clinician.
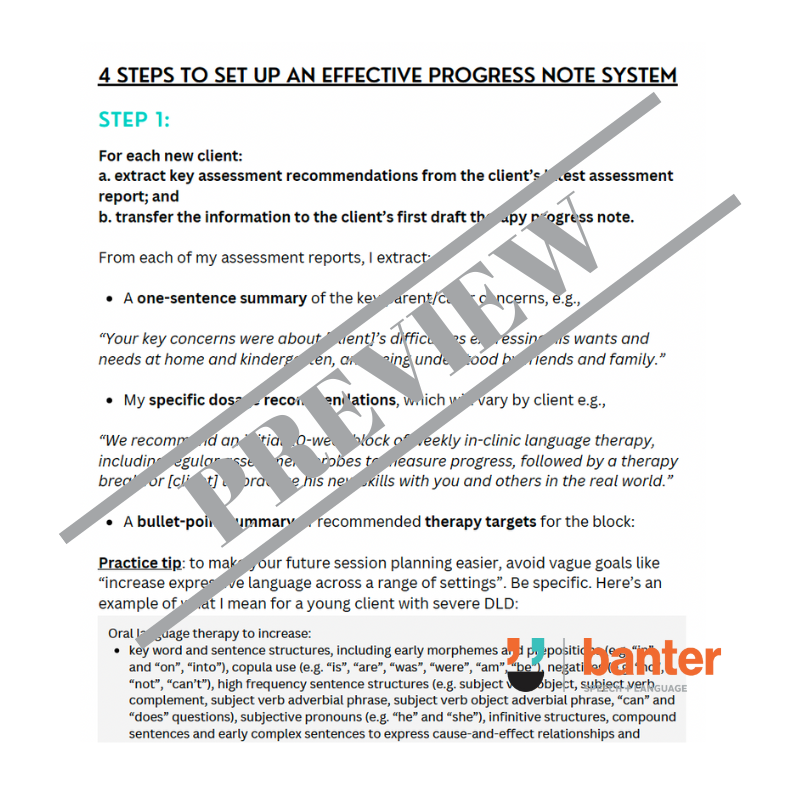
In my own practice, we use a progress note system. For each client, and for every session, we use a system that integrates:
- key therapy recommendations, including goals and dosage;
- home practice recommendations;
- data collection and progress;
- built in-breaks and discharge plans; and
- planning for the client’s next session.
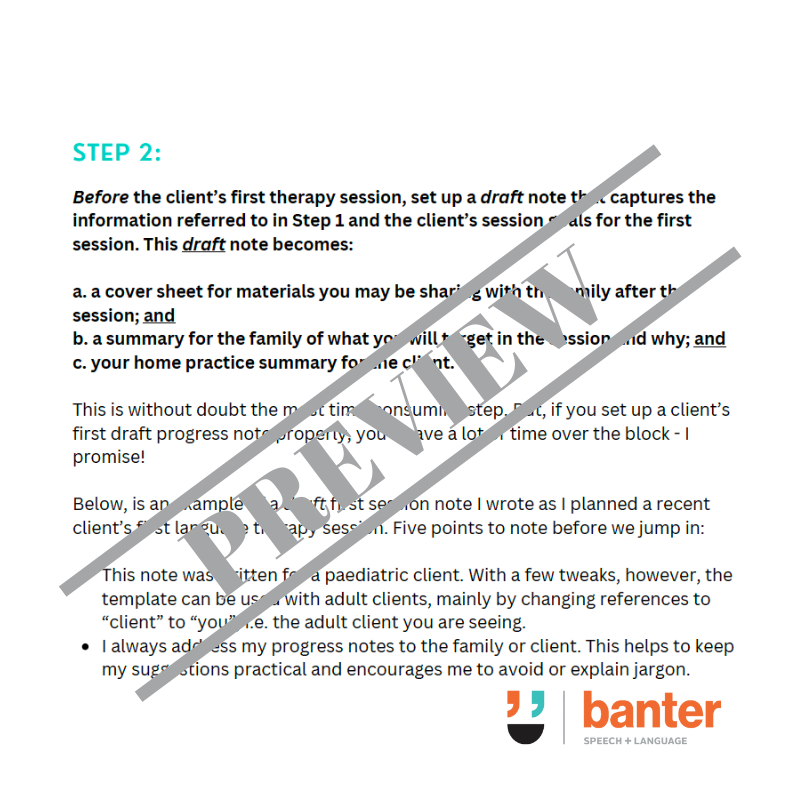
From feedback on our first version of this resource, I know you want a template that’s flexible and platform neutral:
- Almost all of us – even old people like me – write our notes electronically.
- Most of us use practice management systems, like Cliniko or Halaxy.
- Many of us have moved away from the medical model, and want to recognise our clients’ strengths, resources, capabilities as well as their challenges, and want to focus on real world functional and participation goals.
- Many allied health professionals love personalising their progress notes to match their personal style and preferences, and to match the template’s look to their house style. What I focus on here are the content and process of a good progress note. I’ll leave the graphic design to you (or your practice management system).
Our Progress Note System is available as a 15-page PDF (including a worked example) and a 2-page platform-neutral template (Word).





 Gentle debt collection letter pack to recover late payments
Gentle debt collection letter pack to recover late payments